Posts Tagged ‘cervical shortening’
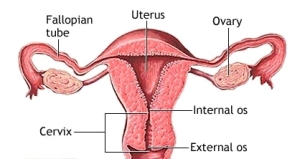
The cervix is the narrow, tubular, lower end of the uterus that extends into the vagina. When you’re not pregnant, the cervical canal remains open a tiny bit to allow sperm to enter the uterus and menstrual blood to flow out. Once you become pregnant, secretions fill the canal and form a protective barrier called the mucous plug. During a normal pregnancy, the cervix remains firm, long, and closed until late in the third trimester. At that point it usually starts to soften, shorten (efface) and open up (dilate) as your body prepares itself for labor.
Normally, in the late second and early third trimester the cervical length measures anywhere between 3 cm to 3.5 cm (30-35mm) and decreases progressively as the pregnancy advances, in preparation for labor (source: Obstetrics and Gynecology Board Review Manual).
In cervical insufficiency, the cervix becomes softer and weaker than normal or is abnormally short to begin with. It may efface and dilate without contractions in the second or early third trimester as the weight of the growing baby puts increasing pressure on it. This condition can sometimes result in second term miscarriage, or premature rupture of the bag of waters, which can then result in preterm labor, especially before the 34th week.
Several studies have indicated that the likelihood of preterm delivery increases with decreasing cervical length. A cervical length of 25–30 mm before 32 weeks gestation seems to increase the risk of preterm delivery. If examination and ultrasound show that you have an abnormally short cervix, and you’re less than 24 weeks pregnant, your practitioner may recommend “cerclage”, a procedure in which she stitches a band of strong thread around your cervix to reinforce it and help hold it closed. However, there’s a lot of controversy about whether cerclage should be used in this situation.
Some recent research questions the effectiveness of the procedure at preventing miscarriage or preterm birth except in a small number of circumstances. And the procedure itself can lead to preterm delivery caused by uterine infection, ruptured membranes, and uterine “irritation” leading to contractions.
In certain other conditions, the benefits of cerclage can outweigh the risks. Women who seem to benefit from cerclage include those who’ve had three or more unexplained second-trimester losses or preterm births. If you’re in this group, you’re likely to get a cerclage at 13 to 16 weeks, before your cervix starts to change. A cerclage done then appears less risky than one done later in pregnancy, after your cervix has started to change. Once this procedure is done, you will be continually monitored by your obstetrician, until about 37 weeks, when the stitches can come out, and you can wait for labor to begin.
If this condition is discovered in the third trimester, bed rest or modified bed rest, would be the preferred choice, as opposed to cerclage. Although there’s no solid evidence that staying in bed is effective, the theory is that keeping the weight of the uterus off of a weakened cervix might help.
After going through a lot of recent research and literature, I have put together some recommendations for expectant mothers who are diagnosed with cervical shortening.
- Women with cervical measurements exceeding 26 mm should be just observed, and reassessed in 2-3 weeks.
- Women with cervical lengths between 21-25 mm should be placed on reduced physical activity, with re-measurement in 2 weeks.
- Women with cervical lengths between 16-20 mm should be placed on strict bed rest, with re-measurement in 1 week.
- Only women with cervical lengths of 15 mm or less should be considered for therapeutic cerclage.
- At this time, no evidence supports measuring cervical length or placing cerclage in the low-risk patient. This means, no scans and no other physical checks or interventions are recommended in the absence of symptoms and/or high risk in the expectant mother.
While this is probably a good point of reference to start, it obviously needs to be taken within the context of the rest of your physical examination findings, and your obstetrician’s recommendations. In addition, your obstetrician will decide what the best intervention is for you, depending upon when your cervical shortening is diagnosed. For more details on this particular topic you can look at information available in the following websites:
As always, please write in any queries, concerns or thoughts that you might have.
Dr. Vijaya Krishnan
UPDATE:
Our Web address has changed. Please visit http://healthy-mother.com and view the various articles, blogs and participate in discussions around pregnancy, newborn care and well woman care.